skip to main |
skip to sidebar
A study found no link between the consumption of aspartame and elevated risks of brain cancer 
A new study on the artificial sweetener aspartame may make diet soda lovers breathe a little easier. A large federally funded study done by government researchers at the National Cancer Institute found no link between the consumption of aspartame and elevated risks of brain cancer and blood-related cancers like leukemia. Aspartame is found in the diet version of popular drinks. Fears about aspartame and cancer have plagued the artificial sweetener since it was first approved by the Federal Drug Administration in 1981 and were inflamed by an Italian study last summer done on rats. That study caused alarm because it showed an increased incidence of lymphoma and other cancers in rats that consumed the equivalent of four to five 20-ounce bottles of diet soda a day for a 150-pound person. In contrast, the National Cancer Institute study, which looked at aspartame consumption among about 567,000 people between the ages of 50 and 69, showed no cause for concern, even among heavy users of aspartame. The Calorie Control Council and the American Beverage Association, both of which represent beverage companies, hailed the study as further evidence that aspartame, despite its bad rap, is a safe food additive. Michael F Jacobson, executive director of the Center for Science in the Public Interest, a nutrition advocacy group that is often critical of the food industry, said that because the study evaluated people aged 50 to 69 and then followed up for five years to check on the incidence of cancer, it may have failed to address the occurrence of cancer for people in their 70s and 80s. Despite that, the findings do take much air out of the idea that aspartame causes cancer.
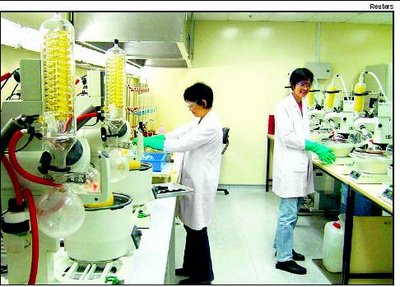
Researchers find that stem cell transplant improves stroke damage 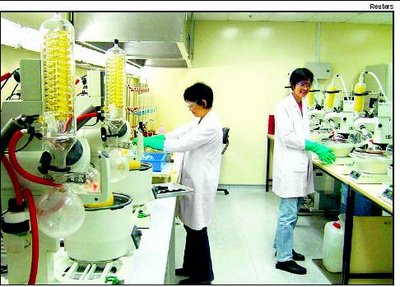
(Picture: STEM CELL TRANSPLANT: Improves stroke damage)
There is now a hope for patients with a neurological damage like stroke. According to a new research, a single dose of adult donor stem cells given to animals that have neurological damage similar to that experienced by adults with a stroke or newborns with cerebral palsy can significantly enhance recovery from these types of injuries. Using a commonly utilised animal model for stroke, researchers administered a dose of 200,000-400,000 human stem cells into brains of animals that had experienced significant loss of mobility and other functions. The stem cells used in the study were a recently discovered type, referred to as multipotent adult progenitor cells, or MAPCs. Treated animals experienced at least 25 per cent greater improvement in motor and neurological performance than controls, Dr Cesario V Borlongan, neuroscientist at Medical College of Georgia and the Veterans Affairs Medical Centre in Augusta said. Dr David Hess, adult stroke specialist, chair of the MCG Department of Neurology and a study co-author said. “It’s a huge public health problem in the world,” said Dr Hess. He says he hopes one day stem cell therapy, along with aggressive physical therapy and possibly tPA can work synergistically to reduce that disability. “These are not going to be cures, but this level of recovery is significant... If somebody can go from a wheelchair to a cane that is a big improvement, that is how we look at it,” Hess said. Adult animals were tested across a range of standardised tasks both before and after undergoing the surgically induced stroke, and measurements were made of their performance. Following the stroke, both control animals and those that received a single injection of stem cells were evaluated for a period of up to two months. Improvements in stem cell treated animals included enhanced performance across the range of tests, which examined strength, balance, agility and fine motor skills, and also included greater recovery of injured tissue. “A single dose of the cells produce robust behavioural recovery at an early period post-transplantation and the recovery was durable, lasting up to two months, which was the entire length of this study,” Borlongan said. “Furthermore, animals continued to show improvement over time.” Even though less than one per cent of the transplanted cells were present two months later, animals receiving treatment developed new neurons, apparently formed from endogenous stem cells. “The mechanism that we are putting forward is these donor cells are secreting nourishing trophic factors that are helping the host brain cells survive and stimulating stem cells from the host to multiply,” Borlongan said. To help mimic potential clinical scenarios for stroke victims, transplants were performed seven days after the initial injury. Currently, ischemic stroke patients may be treated with tPA, the only FDA-approved stroke treatment available, but must receive treatment within three hours from the time the stroke initially occurs. As a result, 95-97 per cent of ischemic stroke victims never receive treatment with tPA. In the adult stroke model, MCG researchers found giving stem cells increased the number of injured cells that survived in the area just outside the area of greatest damage, also referred to as the ischemic core, by 5-20 per cent. Animals in the model of cerebral palsy, a condition caused by an ischemic injury similar to stroke but occurring before or during birth, also experienced at least a 25 per cent improvement over controls. Rodent stem cells were used in this model, a larger per cent of donated cells survived and within two weeks matured into neurons in the young, more pliable brains, Dr Borlongan said. Also, close donor matching seemed unnecessary. Unmatched transplants, from the same species, and genetically identical transplants yielded essentially equal results. Athersys, Inc, a Clevelandbased biopharmaceutical company pursuing cell therapy programs in cardiovascular disease, stroke, cancer and other diseases, funded the research in which previously frozen human or rodent multipotent adult progenitor cells, which the company calls MultiStem, were thawed and injected directly into the brain. Researchers believe that MultiStem cells are able to deliver a therapeutic benefit in multiple ways, for example by producing factors that limit tissue damage and stimulate repair, according to Dr Gil Van Bokkelen, company chairman. In addition, MultiStem cells can safely mature into a broad range of cell types and can be produced on a large scale, something which should ease the move toward clinical studies and eventual clinical use.
© blogger templates 3 column | Make Money Online